A caller requested help interpreting the result of a SASSI-4 questionnaire on a male client who presented himself as having an opioid addiction.
‘Curtis’ is a 36-year-old married man. He and his wife have no children. He works as a landscaper which he describes as physically very demanding. His parents smoked marijuana while he was growing up and Curtis also smokes marijuana. His older brother died ten years ago, and Curtis is still grieving. His brother also had substance use issues. Curtis also may have a history of being molested as a child which he does not remember, but his brother relayed that they were both molested by a babysitter.
Curtis reports a four-year history of opioid addiction which started as a result of a herniated disc in his back. He was initially prescribed hydrocodone for pain. He tried to quit once three years ago. Currently, he is ordering “stuff off the internet” or getting oxycontin from friends. He has been taking 180 mg/day with a maximum of 240 mg per day. It takes 150 mg. for him not to get “sick.” Curtis continues to smoke marijuana on the weekends about one time per week. He has a legal history of possession of marijuana in 2004 and attended an outpatient treatment program doing “what I had to do.”
He has been slowly tapering off the opioids for the past five weeks and currently is down to 80 mg/day. His goal is to completely get off the opioids but he is not interested in residential treatment at this time because it is his busiest time of year. Although he has attended NA, he does not like it. Curtis is more drawn to Smart Recovery.
The SASSI-4 was administered for lifetime use on the face valid side of the questionnaire.
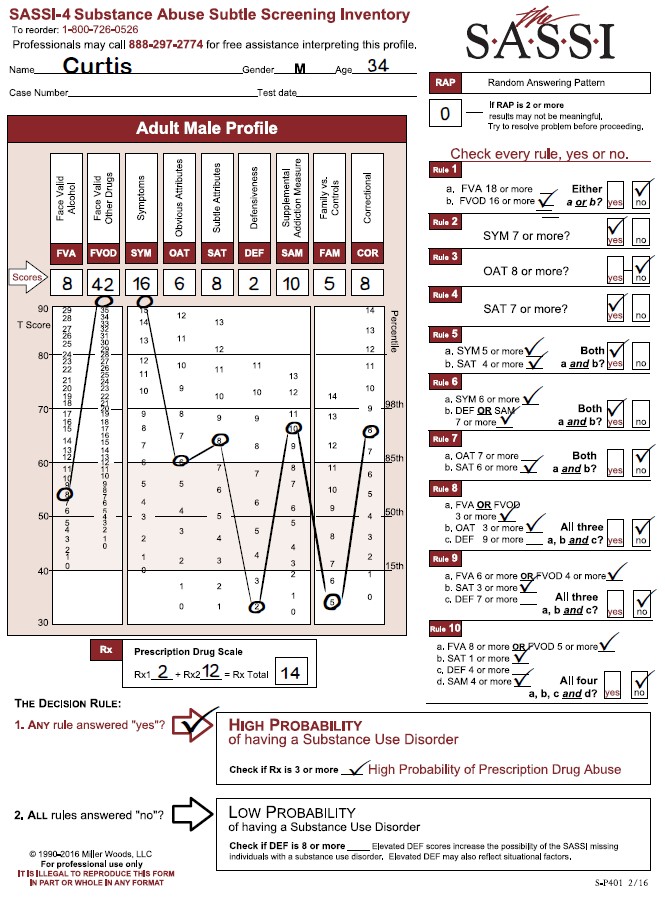
What were his SASSI-4 results? Curtis has a ‘High Probability of having a Substance Use Disorder’ and a ‘High Probability of Prescription Drug Abuse.’
This looks like a straightforward profile on the face of it. His score of 42 on the FVOD and 18 on the SYM indicate someone who is very open concerning his drug use, and because these are face valid scales, content analysis could provide useful information to further explore with the client.
The OAT score of 6 is right at the 85th percentile. The client may be able to identify with some of the characteristics of substance users such as impatience, resentment, self-pity and impulsiveness. However, the SAT score of 8 is higher than the OAT and may blunt the ability for Curtis to have insight into his behavior. When the SAT is higher than the OAT, the client may exhibit a lack of awareness or simply denial around the impact drugs are having on his life. In this case and not unusual, opioid users do not see themselves as “typical” addicts. That may account for the OAT score.
The DEF score of 2 can be a ‘red-flag’ as it is below the 15th percentile. A score this low can indicate someone with poor ego strength, feeling helpless and hopeless and may be exhibiting symptoms that look like depression. The clinician may want to do a mental health screening or refer the client for screening.
The FAM score of 5 is also very low, below the 15th percentile. This can indicate the client is focused on himself and not that concerned about others. This does not indicate a personality disorder but given the client’s circumstances, makes sense that he would be more internally focused.
The COR score of 8 is elevated above the 85th percentile. He has answered in a similar way to people who have had legal issues for any reason. We suggest screening for those behaviors or characteristics we often see in that population. These can range from poor social skills, low frustration tolerance, risk-taking behaviors, anger management issues or impulse control issues. These issues could be impacting on Curtis’s choice-making abilities.
Finally, looking at the Prescription Drug Scale. With the score of 14, it is quite clear that he is identifying behaviors associated with prescription drug abuse. Again, as a face valid scale, looking at these individual items will generate a lot of information for the clinician. The clinician will need to look at treatment readiness, discuss medication needs, possible referral and other reported clinical issues.
PDF Version Available for Download
Thank you for reading this post, don't forget to subscribe!