The Importance of Additional Assessment Data
The client is a 38-year-old male named Jim (not his real name), who was referred for a substance use evaluation following a second arrest for domestic violence. The practitioner calling in the profile reported having collateral evidence substantiating a significant history of alcohol abuse for this client.
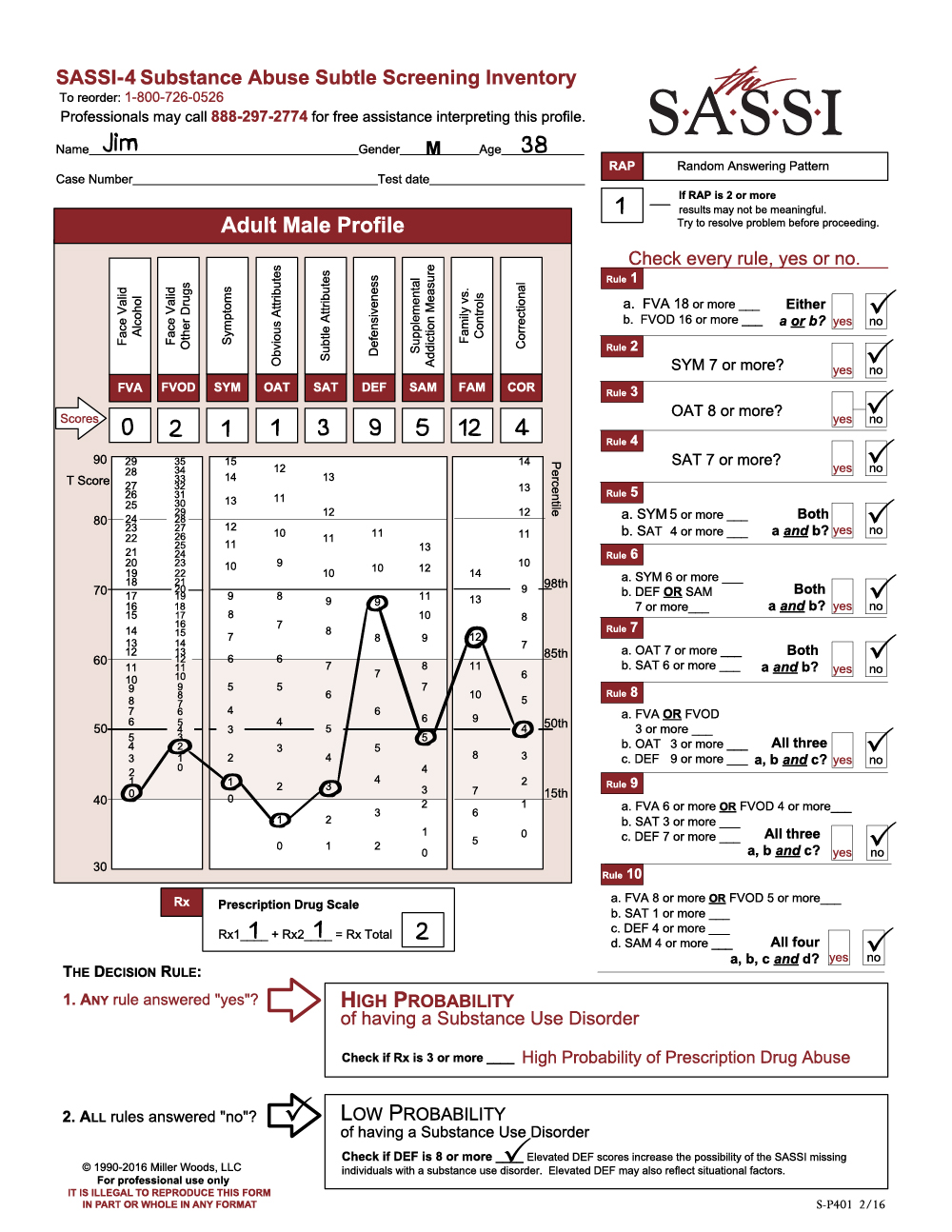
The SASSI results indicate that Jim has a low probability of having a substance use disorder. He is not acknowledging any significant problematic use of alcohol (FVA=0) or other drugs (FVOD=2). In fact, he denies having any of the symptoms commonly associated with individuals who have substance use disorders (SYM=1). However, note that Jim’s responses are highly defensive (DEF=9) and significantly similar to individuals who are instructed to minimize and conceal problems. Given that his report on the FVA and FVOD is in direct conflict with information from other sources, it is likely that he is minimizing the degree to which he has experienced alcohol and other drug problems or related symptoms. This increases the risk that the SASSI classification of low probability may be in error – in other words, the accuracy of the decision rules may be slightly decreased. As in most assessment situations where the client is relatively defensive, augmenting self-reported alcohol and drug history with data from external sources is advisable before ruling out substance use problems.
Experienced SASSI users working in criminal justice, EAP, DOT, child protection, and other similar settings will recognize this profile as relatively common for clients who are mandated for assessment. Indeed, Jim has been charged with assaulting his partner for a second time. One possibility is that he fears a harsh punishment may be coming if he does not present himself in a favorable way. He may also be convinced that he is not to blame for his behavior, explaining that his partner provoked him or that he was acting in self-defense. While the SASSI does not reveal the exact cause or reason, the high DEF score is a strong indicator that Jim approached the assessment in a defensive manner.
Notice also that Jim’s OAT score is significant given that it falls below the 15th percentile (OAT=1), meaning that only 15% of the general population would score this low. A score in this range usually indicates a person does not identify with any of the problematic behaviors typically associated with substance abuse (for example, anger management problems, negativity, self-centeredness, etc.). Jim is not likely to acknowledge having these behaviors and probably wants to be viewed as being completely different from people who do. Individuals with a family history of addictive or violent behavior often cope by distancing themselves from the addict or perpetrator as if to say, “I’m nothing at all like my alcoholic mother or physically abusive father.” In fact, the caller reported that Jim’s mother is an active alcoholic.
Jim’s FAM score of 12 is also significantly elevated (above the T 60 line or the 85th percentile). His responses are similar to family members of substance dependent individuals. It is likely that he shares many of the characteristics and traits commonly associated with individuals living in addictive family systems – obsession with controlling the thoughts, feelings and/or actions of others, lack of adequate or healthy psychological, emotional and physical boundaries in relationships, and inability to trust others. Certainly, one theme for individuals with high FAM scores involves their sense of happiness and self-worth being dependent on fixing or controlling the behavior of others. Jim may have learned early on the false perception that the only way he can have a sense of well-being is when he is in complete control of his partner. This need often can result in the perpetration of violence in cases where poor interpersonal boundaries and lack of trust exist in a person with serious impulse control problems. Thus, like other perpetrators of domestic violence, Jim may feel enmeshed at every level with his partner, seemingly unable to restrain himself when he feels like he is losing control of his partner’s behavior.
To summarize, Jim’s profile is similar in many ways to that of other known perpetrators of domestic violence who have completed the SASSI. Although he is classified as having a low probability of a substance use disorder, his responses are characterized by a significant degree of defensiveness. This, along with other assessment evidence, increases the risk that he has minimized his alcohol and other drug problems and that the SASSI results of low probability of substance use disorder may be inaccurate. Jim does not recognize or accept responsibility for his own behavioral problems. Like other domestic violence offenders, he tends to focus almost exclusively on controlling his partner’s behavior as a way of achieving happiness and contentment in life. Jim’s family history of alcoholism is likely a significant contributor to his behavioral problems and also increases the risk that he may have, or may be developing, a substance-related disorder.
Ongoing assessment will be necessary to completely rule out the possibility of a substance use disorder. Because of the impact that most psychoactive substances tend to have on reducing impulse control, Jim’s risk for reoffending is greatly increased if he has a substance-related disorder that is left untreated. Collateral sources of information concerning Jim’s alcohol and drug history seem to indicate that his problems with alcohol and other drugs may be more serious than he is reporting on the SASSI. If further assessment results confirm a diagnosis of a substance use disorder, his treatment plan would need to include some form of addictions therapy. In addition, a no-use contract and regular toxicological screens could be useful ways to lower his risk of using and support a period of abstinence.
Jim’s defensiveness could be a serious barrier to engaging him in a therapeutic relationship, let alone making any significant progress in helping him to change any of his problematic behaviors. Establishing rapport and gaining Jim’s trust and confidence would be important steps in creating and maintaining a therapeutic alliance with him. Didactic, cognitively based educational approaches are often viewed by defensive clients as less intrusive and non-threatening. Initially, he may respond more favorably to presentations, films, books, etc., emphasizing the impact of addictions on the individual and their families. This may help to increase Jim’s awareness of his own misuse of substances and provide him with some insight into the dynamics of his own family’s behavior, including his alcoholic mother. Family involvement in his treatment may also be beneficial.
Referral to a practitioner or program that specializes in treating perpetrators of domestic violence should be strongly considered. Remember that Jim may have little or no awareness that he is responsible for his own violent behavior. His perceptions may be completely dominated by the belief that he has a right to behave in this manner with his partner. Such deeply ingrained patterns of thought and associated impulse control problems are often difficult for clients to begin to recognize, much less change. Support and process groups facilitated by behavioral health professionals trained in the treatment of domestic violence offenders are often an effective approach in helping perpetrators begin to acknowledge their behavioral problems and to effect some healthy changes.